Dysfunctional Synaptic Function Is Key to Schizophrenia
- Get link
- X
- Other Apps
Summary: Schizophrenia itself is associated with loss of excitation, but hallucinations and other symptoms of the disorder are caused by a loss of synaptic inhibition.
Source: Elsevier
Schizophrenia, which can cause disrupted thought and mood, delusions and hallucinations, is among the most debilitating mental disorders and the most mysterious.
Researchers have long suspected that the symptomology of schizophrenia fundamentally arises from disrupted synaptic function, or abnormalities in the way that neurons communicate with one another, perhaps leading to an imbalance between excitatory and inhibitory transmission.
Now, a new study has shown that schizophrenia itself is associated with a loss of excitation, but hallucinations and other symptoms are associated with a loss of inhibition.
The study appears in Biological Psychiatry.
The authors, led by Rick Adams, PhD, at University College London, used electroencephalography (EEG), a noninvasive technique that measures brain waves, to collect data from 107 participants with a diagnosis of schizophrenia, 57 of their relatives and 108 control participants. The EEGs of people with schizophrenia displayed hallmark signs including increased theta waves.
“The nature of brain circuit changes in schizophrenia is unclear,” said Dr. Adams. “Is it too much excitation or not enough, or too much inhibition or not enough, or some combination?”
To find out, Dr. Adams and colleagues used computational modeling of the EEG data, which showed that the EEG differences seen in people diagnosed with schizophrenia resulted from decreased synaptic gain. This means that excitatory neurons had a diminished ability to stimulate one another.
Symptoms of schizophrenia including auditory hallucinations, however, were associated with a loss of neural inhibition, especially in auditory brain areas.

“This might mean that the loss of excitation comes first, and the brain tries to compensate for this by reducing inhibition, but then this leads to hallucinations,” Dr. Adams said.
“Imagine you are trying to listen to someone speaking on the radio, but the signal is very weak; if you turn the volume up, the speech is louder–but so is all the static and background noise–and so you may mistake some of this noise for actual speech. Something analogous might be happening in brain circuits in schizophrenia.”
John Krystal, MD, Editor of Biological Psychiatry, said of the work: “Working out the fundamental features of synaptic dysfunction in schizophrenia may help to guide both pharmacological and neurostimulation treatments for this disorder.”
About this schizophrenia research news
Author: Rhiannon Bugno
Source: Elsevier
Contact: Rhiannon Bugno – Elsevier
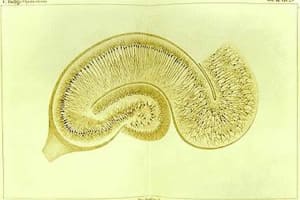
Image: The image is in the public domain
Original Research: Open access.
“Computational modelling of EEG and fMRI paradigms indicates a consistent loss of pyramidal cell synaptic gain in schizophrenia” by Rick Adams et al. Biological Psychiatry
Abstract
Computational modelling of EEG and fMRI paradigms indicates a consistent loss of pyramidal cell synaptic gain in schizophrenia
Background
Diminished synaptic gain – the sensitivity of postsynaptic responses to neural inputs – may be a fundamental synaptic pathology in schizophrenia. Evidence for this is indirect, however. Furthermore, it is unclear whether pyramidal cells or interneurons (or both) are affected, or how these deficits relate to symptoms.
Methods
Participants with schizophrenia diagnoses (PScz, n=108), their relatives (n=57), and controls (n=107) underwent three electroencephalography (EEG) paradigms – resting, mismatch negativity, and 40 Hz auditory steady-state response – and resting functional magnetic resonance imaging. Dynamic causal modelling was used to quantify synaptic connectivity in cortical microcircuits.
Results
Classic group differences in EEG features between PScz and controls were replicated, including increased theta and other spectral changes (resting EEG), reduced mismatch negativity, and reduced 40 Hz power. Across all four paradigms, characteristic PScz data features were all best explained by models with greater self-inhibition (decreased synaptic gain), in pyramidal cells. Furthermore, disinhibition in auditory areas predicted abnormal auditory perception (and positive symptoms) in PScz, in three paradigms.
Conclusions
First, characteristic EEG changes in PScz in three classic paradigms are all attributable to the same underlying parameter change: greater self-inhibition in pyramidal cells. Second, psychotic symptoms in PScz relate to disinhibition in neural circuits. These findings are more commensurate with the hypothesis that in PScz, a primary loss of synaptic gain on pyramidal cells is then compensated by interneuron downregulation (rather than the converse). They further suggest that psychotic symptoms relate to this secondary downregulation.



Comments
Post a Comment